Diabetic foot ulcers are one of the major complications of diabetes. Between 19 and 34% of all diabetics will develop a foot ulcer at some point in their lives (1). Often underestimated, or even unrecognised by the patients affected, it can lead to complications such as an infection requiring hospitalisation, or even in the worst cases, amputation. After amputation, patient life expectancy does not exceed 5 years in almost 70% of cases, which is lower than that for certain types of cancer (2). This outcome is not however a fatality. With proper prevention, ulcers can be avoided.
What causes diabetic foot ulcers?
Diabetes does not only cause blood sugar imbalance. It also causes two phenomena which increase the risk of occurrence of a diabetic foot ulcer:
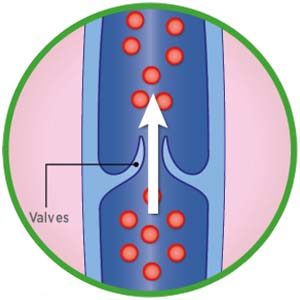
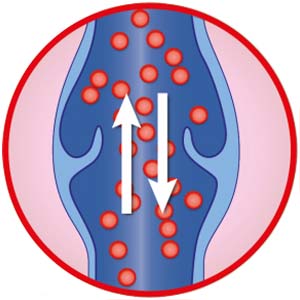
- Involvement of the distal nerves of the legs, especially with loss of sensitivity. As a result, the patients only rarely feel they have an ulcer (neuropathic ulcer).
- Blocked arteries, ultimately leading to insufficient blood flow (ischemic ulcer).
In three out of four cases, diabetic foot ulcers are related to wearing uncomfortable shoes, to an injury caused when cutting the toe nails, to a burn/friction or to fissures / cracks on the soles of the feet.
The longer an ulcer remains open, the more the risk of infection increases. It can lead to amputation in extreme cases.
What is a diabetic foot ulcer?
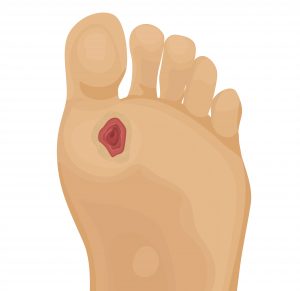
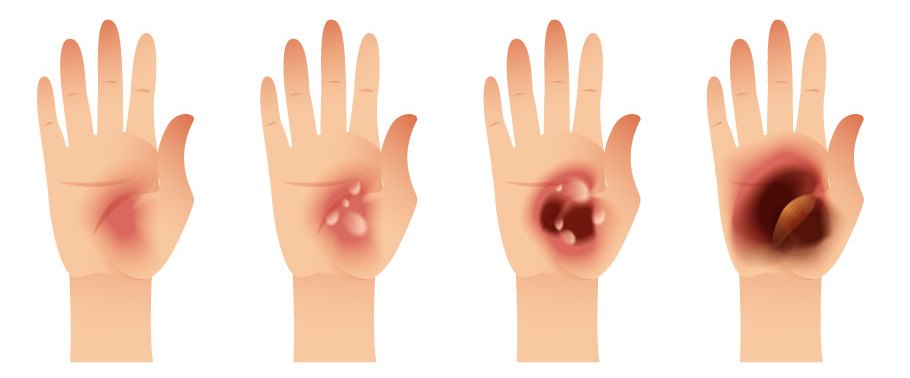
Caused by an initially minor lesion (a simple cut through to wearing uncomfortable shoes), a diabetic foot ulcer can take three forms:
- Neuropathic ulcer. Appearing on the toes or under the arch of the foot, as a perforating ulcer of the foot, on the foot joint, this ulcer begins with a callus or corn. It comes with a loss of sensitivity (pain/heat), has clear edges and the skin is dry. In effect, diabetes causes neuropathy which affects the sensory and motor nerves, weakening the extremities of the lower limbs. Therefore the patient’s foot becomes deformed and their nails become curved like claws. The loss of sensation in the foot can even prevent the patient feeling they have an ulcer, which can then rapidly become infected.
- Ischemic ulcer. This is related to a perfusion defect. It mainly occurs on the tips of the toes, on the heel or edge of the foot. The skin breaks, and is pale or bluish in colour. The foot is cold and painful, and the patient can feel burning or itching sensations. Yellow, red, pink, or even black if it is necrotic, the ulcer can take on different colours, depending on its stage of progression.
- Neuroischemic ulcer. It is related to neuropathy and is associated with The ulcer forms on the edge of the foot or tips of the toes, or even under the toenails. The first sign is generally a blister caused by repeated friction of the foot in shoes that are too tight or too narrow.
In adults, an infection is likely to occur in addition to the ulcer. In effect, the open wound is subject to bacterial invasion. Diabetic foot ulcer therefore makes diabetes the leading cause of amputation in the world3.
Diabetic foot ulcer prevention
The severity of the foot involvement requires targeted prevention according to the risk. The Haute Autorité de Santé (HAS)4 has therefore defined a podiatric risk grading system in order to adapt treatment. The foot assessment is used to grade the level of risk according to the following classification:
Grade 0: no sensory neuropathy
Podiatric risk grade 0 means there is no loss of sensitivity in the feet. Therefore, the risk is the same as in the general population. It is the most common situation. Standard hygiene rules should be followed, like wearing appropriate, non-traumatic footwear or avoiding maceration (feet should be dried properly and synthetic socks should be avoided) and traumatic treatments (e.g.: use of a scalpel). It is especially important to balance the diabetes as far as possible and to control any risk factors (e.g.: smoking, arterial hypertension, cholesterol etc.).
Grade 1: isolated sensory neuropathy
In addition to the recommendations that apply for grade 0, you can also follow the advice below:
If the ulcer is very painful or uncomfortable, talk to your doctor about it. Certain medicines can provide relief, in addition to balancing blood sugar.
If the ulcer involves loss of sensation, you or a member of your family must inspect your feet daily. It will enable you to detect any ulcers that go unnoticed. It is essential to see a doctor as soon as possible if there is an ulcer, even if it is not painful.
It is especially important to not damage the feet using too abrasive and/or corrosive treatments, by wearing shoes that hurt or walking barefoot etc. Apply a moisturising cream daily if your feet are very dry. Of course, your diabetes should be controlled as effectively as possible to prevent the neuropathy worsening.
Grade 2: sensory neuropathy with arteriopathy of the lower limbs and/or foot deformation
Grade 3: history of ulcer or amputation
These very high risk feet (grade 2 and grade 3) require both increased vigilance on your part and/or by your family, but also active ulcer prevention measures. Podiatrists or nurses can remove the hyperkeratosis (callus). Podiatrists/chiropodists/orthotists can make ortheses or insoles to correct abnormal weight bearing areas. Sometimes, if your foot is very deformed, you may even have to wear specially-made shoes. If there is arterial involvement, revascularisation may be essential.
Good to know !
Two types of prevention can be paid for on prescription for diabetic patients with podiatric risk grade 2 or 3:
- a yearly preventive treatment for grade 2 risk foot lesions. It includes 4 prevention sessions per year maximum;
- a yearly preventive treatment for grade 3 risk foot lesions. It includes 6 prevention sessions per year maximum.
The prevention treatments dispensed at the patient’s home must come with a medical prescription to be reimbursed.
The yearly prevention package includes an initial foot assessment, prevention sessions and a brochure.
Treatment
First of all, diabetic foot ulcers require rapid and comprehensive treatment to minimise the risk of complications. Regardless of its size, the ulcer must then be closely monitored by a multi-disciplinary team. The team includes the diabetes specialist, the general practitioner, the nurse, the podiatrist-chiropodist and the surgeon who will all closely monitor the more or less rapid progress of the ulcer.
Wearing a pressure relief device is also compulsory. It means the foot does not press on the ulcer and more effectively distributes pressure on walking, so as not to aggravate the wound.
It is essential to apply a dressing after careful ulcer cleansing and removal of denervated tissue. Its aim is to promote healing.
The diabetes, comorbidities and nutritional status must also be managed at the same time.
And afterwards?
70% of healed diabetic foot ulcers relapse within 5 years5 . Diabetic patients must therefore take special care of this part of their body, by following some basic recommendations:
- Wear shoes suited to the shape of the foot, and always with socks.
- Never walk barefoot
- Show their feet to a chiropodist on a regular basis
- Monitor the general foot condition (use a mirror to inspect the sole)
- Continue to closely monitor blood sugar levels and follow a diabetes-reducing diet.
- Ask a podiatrist or chiropodist to look after their feet and nails (cutting/filing) and not use corn remover (product to remove corns)
- Wash their feet daily with soap and water, not forgetting to dry between the toes and user a moisturiser to keep them supple.
- Not warm their feet using a heat source (e.g. Hot water bottle)
1- Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med 2017; 376: 2367-75
2- Walsh JW, Hoffstad OJ, Sullivan MO, Margolis DJ. Association of diabetic foot ulcer and death in a population-based cohort from the United Kingdom. Diabet Med 2016; 33:1493–98.
3- Whiting, D. R., Guariguata, L., Weil, C., and Shaw, J. 2011. “IDF Diabetes Atlas: Global Estimates of the Prevalence of Diabetes for 2011 and 2030.” Diabetes Res. Clin. Pract. 94 (3): 311-21.
4- Evaluation of the acts performed by the pedicure-podiatrist for the prevention of grade 1 risk foot injuries in the diabetic patient. French Health Authority. (Évaluation des actes réalisés par le pédicure-podologue pour la prévention des lésions des pieds à risque de grade 1 chez le patient diabétique. Haute Autorité de Santé)
5- Connor H, Mahdi OZ. Repetitive ulceration in neuropathic patients. Diabete
- an ulcer
- a scratch
- a cut
- a blister
- feel pain
- swelling
- redness
Treatment of diabetic foot ulcers
It’s really important to contact you GP, podiatrist or nurse immediately if you see something wrong – no matter how small the wound.
The important thing to remember is to keep your weight off your foot.
A key factor to close the wound and to avoid complications such as infection and amputation is to react early. It is important that your feet are being taken care of by a team of specialists
For more information on Diabetic Foot Ulcer please visit Save Feet Save Lives